Acton: Measures Will Prevent Two-thirds of Coronavirus Deaths
YOUNGSTOWN, Ohio — The Ohio Department of Health will issue an order defining what procedures should be prioritized over the next few weeks as the state continues to navigate the coronavirus outbreak.
The order will be consistent with the current understanding about surgeries and other activities taking place in hospitals so as to preserve personnel, bed space and personal protective equipment, Gov. Mike DeWine said.
The order will prioritize surgeries that are life-saving; preserve the function of an organ or preserve a limb for a patient; will reduce the spread of disease or metastasizing of cancer; or reduce the risk of progression of severe symptoms.
“Anything that fits into these categories … will still be able to be done,” said Dr. Andy Thomas, chief clinical officer for the Wexner Medical Centre at Ohio State University. Thomas represented the medical advisory group from the Ohio Hospital Association, which worked with the Ohio health department to craft the guidelines with direction from the U.S. College of Surgeons and the U.S. Surgeon General. The objective was to define what cases could be safely delayed with no harm, he said.
The order was among several topics discussed during a news conference Tuesday during which state officials provided an update on the coronavirus outbreak.
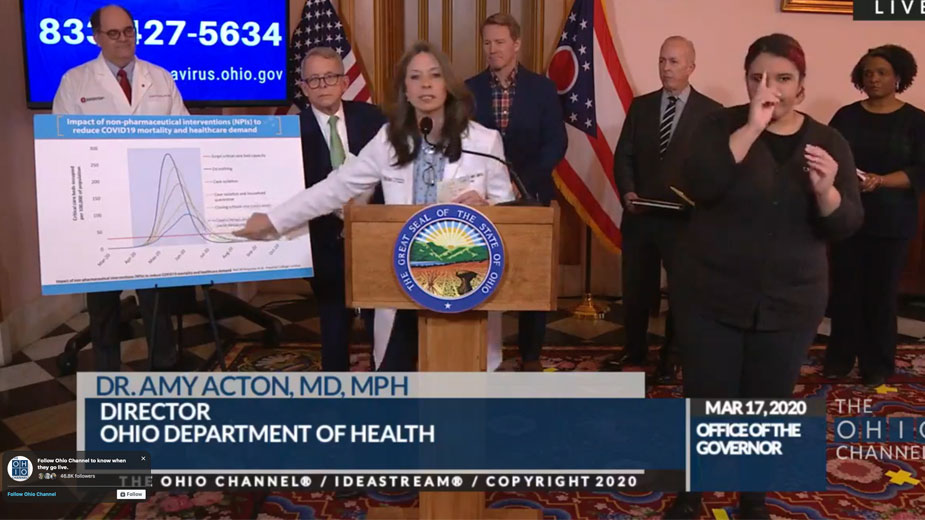
Dr. Amy Acton emphasized that measures taken thus far to prevent the spread of the novel coronavirus “really are going to get us through it a lot sooner,” and in a better way.
Acton, director of the Ohio Department of Health, addressed the familiar curve showing the goals for community mitigation during the coronavirus pandemic. “Timing is everything,” she says, and what is being done is making a difference.
“If we did nothing, we would see that scary, sharp, steep incline that we saw in Wuhan,” Acton says.
A study by Dr. Neil Ferguson with Imperial College in the United Kingdom that outlines nonpharmaceutical interventions to reduce COVID-19 mortality and the demand on the health-care industry led to some of those measures at the federal and state level, Acton said. Those measures include voluntary quarantine, case isolation in the home, social distancing and closure of all schools and universities, as well as limiting gatherings to fewer than 10 in a room.
To abide by the latter, Tuesday’s press conference was held in the state room in the capitol building in Columbus, with a portion of the media split in another room.
Based on earlier studies with no intervention, Acton expected the pandemic would peak in mid-May, she said. Through intervention, the timeline is longer, she acknowledged, but the number of cases are fewer, thus putting less of a strain on health care professionals and health systems, she said.
Flattening the curve ensures the state and the country won’t see the type of spike that Italy is seeing so “we’re not in a situation where we’re overrun” and don’t have the equipment or personnel to meet the need.
“We have to extend the time and slow the spread because that decreases the peak,” Acton said. “There’s no scenario where there won’t be a surge. But if we did nothing, estimates were 2.2 million Americans would die. But taking these measures can cut that by two-thirds.”
Those deaths aren’t just from the COVID-19 strain itself, she explained, but also people who need the hospital for other reasons like having a baby or getting sick.
“It’s all these ripple effects that we’re having. That is why what you’re doing makes all the difference,” Acton said.
Capacity among all Ohio hospitals is “a little less than 75%” and can safely surge another 25% “without doing anything extraordinary at all,” said Mike Abrams, president and CEO, Ohio Hospital Association. That is about par for the course this year because of influenza.
“While this is a difficult situation, the health care infrastructure in the state of Ohio is quite strong,” Abrams said.
To increase capacity, state hospitals have begun thinking outside of the box and have been in talks with area hotels that could deploy a floor to bring in noninfectious patients “who could be safely cared for,” he said. Health care leaders are also in discussions with local leaders about reopening hospitals that have been recently closed.
The federal government has also relaxed rules that limit the state’s 33 critical access hospitals to 25 beds and 96-hour stays, he noted.
Having enough ventilators, beds and personal protective equipment, or PPE, for health care providers is a concern, Acton said.. She thanked dentists and veterinarians in the state for forgoing certain unnecessary procedures to free up their supply of PPE.
“Conservation of PPE is paramount,” added Tamara McBride, chief of the Bureau of Health Preparedness with the Ohio Department of Health. Each state has been allocated a certain amount of PPE from the federal government, and what was allocated for Ohio is “not enough,” and she doesn’t anticipate the state will receive any more, she said.
“[Conservation is] one of the critical mitigation steps that we have to take to ensure that we have the health care professionals in place to go in to leverage those hospitals or hotels that Mike Abrams talked about,” she said.
At the same time of the conference, Mahoning County Public Health confirmed two people in the county have tested positive for COVID-19. One resident is hospitalized, the other is not.
As of this posting, the Ohio Department of Health reports 67 confirmed cases in the state with 17 hospitalizations.
The affected age range is 14 to 86 years old, with the median age of 48, Acton said.
Copyright 2024 The Business Journal, Youngstown, Ohio.