Amid Record Hospitalizations, Providers Urge Ohioans to Pull Back
CEDARVILLE, Ohio — With a record 5,060 patients in Ohio hospitals battling COVID-19, health-care providers are again imploring Ohioans to abide guidelines when in public, and to stay home and reduce contact with others when at all possible.
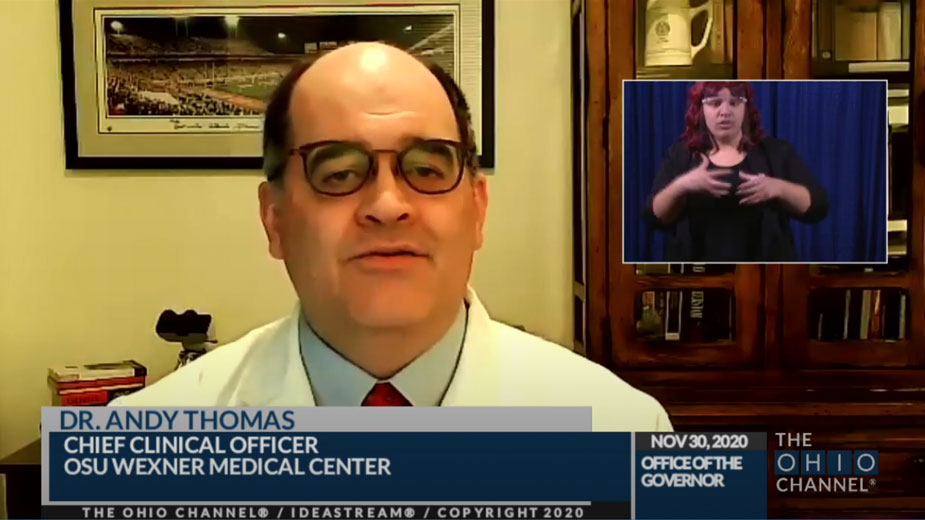
During a coronavirus update Monday with Gov. Mike DeWine, Dr. Andy Thomas, chief clinical officer for The Ohio State University Wexner Medical Center, said capacity and staffing issues for Ohio hospitals are “becoming quite serious.”
On Nov. 1, hospitals in Ohio collectively had just under 1,700 in-patients who were there for COVID-19, he said. The record number on Monday means hospitalizations have increased statewide by 200% since the start of the month.
In Zone 2, which covers central Ohio counties and up toward the northwestern part of the state, hospitals have 1,087 COVID-19 patients, up from just under 400 on Nov. 1, a 177% increase, he said.
“What we’ve continued to see in our zone is the rural areas being hit particularly hard by this,” Thomas said. “Between 40% and 50% of their patients who are in ICU or on ventilators are there because they have COVID. It’s a significant issue that we’re concerned about with ICU capacity.”
At the current rate, patients with COVID-19 will begin “crowding out” patients who don’t have the virus but still need ICU or ventilator care, Thomas said. Currently, a third of ICU patients have COVID, as do a third of those on ventilators.
Smaller hospitals and rural community hospitals don’t always have the ability to expand their ICU capacity, he noted, and many hospitals in the state are delaying some non-urgent surgeries that would result in a patient needing an ICU bed to recover.
Other issues of capacity are being felt as well. A hospital in the northern part of the state recently called in a refrigeration truck because it had exceeded its on-site morgue space, he said.
As hospitalizations have spiked over the past three weeks, it has taken a toll on doctors, nurses and hospital staff as well, said Stacey Morris, COVID unit nurse manager at Cleveland Clinic Akron General. She asked viewers to take the pandemic seriously, adding that it isn’t a hoax, nor is it “blown out of proportion,” she said.
“Our numbers have just risen so quickly and so drastically,” Morris said. “We’ve had to work to triage our beds to make space for the patients and make sure that we have enough room for them. That includes medical, surgical and ICU beds.”
One of the most difficult things to experience has been watching how fast patients can deteriorate, she said. Some have come to the hospital needing just a few liters of oxygen, but that can increase to much more oxygen and possibly an ICU bed within a matter of hours, she said.
The progression and the unpredictability of the virus have been scary, she said. She’s had patients in their 30s and 40s with no health history doing “really poorly” with it. And while there are some treatments, “there’s no magic bullet to treat this right now.” Each day, there are two or three patients in the medical unit who are not doing well, she noted.
Because there are no visitations, caregivers do their best to go into a patient’s room with an iPad so they can speak with their loved ones, she said. The conversations are difficult for the patient and family members, but they also take an emotional toll on the caregiver.
“Typically those are private conversations that happen amongst loved ones,” she said. “And we’ve become a part of that.”
As more people are hospitalized for the virus, “there’s only so many of us to give that care,” she said.
“You can always get more equipment, build more space, put in more beds, but there’s not just hundreds of thousands of nurses and doctors and respiratory therapists just waiting in the wings,” she said. “We’ve been trained for years medically to care for patients at high acuity levels that they have right now with this virus, and you can’t replicate that. You can’t just snap your fingers and make more caregivers appear.”
When talking with ICU patients, nurses will ask the individuals where they think they contracted the virus, said Dara Pence, ICU nurse manager at OhioHealth Riverside Methodist Hospital, Columbus. Typical answers include graduation parties, baby showers, funerals and weddings, Pence said.
“Several of them said, ‘I had a mask, but I put it in my pocket when I saw that everyone else didn’t have a mask,’ ” she said.
Pence echoed Morris’ message about the community needing to take things seriously and follow the guidance. She encouraged people to go out and stock up on what they need to avoid having to go out as often as they usually do, saying that she’d rather see the community run out of toilet paper than see hospitals run out of ICU beds.
“We here at the hospital are no longer the front line,” she said. “We’re a last line of defense. The front line now is the community.”
For those who may have traveled for the Thanksgiving holiday, Wexner’s Thomas advises them they could risk transmitting the virus to friends and coworkers should they be currently asymptomatic. He recommends minimizing contacts as much as possible for five to seven days, including taking some additional time off work, to help break the chain of transmission.
Gov. DeWine agreed and asked employers and employees to continue working from home when possible. For those who have returned to the office over the summer, he asked them to “take a hard look at this and see if they can go remote again.”
In an effort to set the pace, DeWine said the state is putting on hold the Jan. 4 timeframe when it planned to start bringing back state employees in stages who have been working from home.
Ohio is also rolling out a new $28 million COVID-19 Indoor Air Quality Assistance Program to help nursing homes, assisted livings and adult day centers improve indoor air quality during the pandemic. Eligible recipients can receive up to $15,000 to improve indoor air quality through HVAC inspections, portable air-filtration systems, new filtrations systems, maintenance on existing systems and other interventions.
The program is made possible by Cares Act funding.
The program will be managed by the Ohio Bureau of Workers’ Compensation and the Ohio Department of Aging will be working with those businesses to promote the funds. For more information on eligibility requirements and how to apply, visit BWC.ohio.gov.
On Thursday, the governor will give a complete report on when the state can expect to see its first shipment of COVID-19 vaccines. Pending final approval, doses of Pfizer’s vaccine can come as early as Dec. 15, and Moderna’s vaccine Dec. 22.
Copyright 2024 The Business Journal, Youngstown, Ohio.