YOUNGSTOWN, Ohio – Whether it’s providing surgical reconstruction or simply medication to treat pain, orthopedic care is a booming segment of the region’s medical sector, which is the area’s fastest-growing economic sector. To keep up with demand, professionals in the field are looking to the future for new treatments and to other medical fields to bridge the continuum of care.
The ultimate goal of orthopedic care is to minimize the invasiveness of procedures and get patients back to their normal lives as quickly as possible. In most cases, that means avoiding the operating room. Although surgical options such as joint replacements or procedures to repair torn muscles are among the high-profile means of orthopedic care, they’re likely to be the last resort.
“If you have arthritis … it’s on a continuum. When it’s pure arthritis, we can’t cure it because it’s a degenerative process,” says Dr. Kenneth Jones, an orthopedist at Trumbull Regional Medical Center. “You start with medication then move to injections like cortisone or gel shots and you work up treatment from there. The end game, at the very top, is knee replacement.”
Determining the best course of treatment starts with the initial meeting with a patient. Dr. Thomas A. Joseph, an orthopedist and partner at Youngstown Orthopaedic Associates, says he and his colleagues split their time evenly between the office and the operating room at Orthopaedic Surgery Center.

“If a patient has symptoms they want evaluated – it could be pain, swelling, motion restriction – they present to an office,” he says. “Hopefully at the end of that [office] interaction, you have established a diagnosis and treatment plan. Our office visits usually end with a summary and some patient education. We want them to understand what it takes to get better. The first step is nonoperative in most cases, unless you’re dealing with a broken bone or a ruptured tendon or a ligament that needs repaired.”
Some orthopedic issues can be treated with medication, lifestyle changes such as a change in diet or disease management, or physical therapy. But such options aren’t always going to completely solve the issue, says Dr. Louis Lyras, chief of surgery and co-founder of Southwoods Health.
“When you see an orthopedist, they’ll do the more conservative things first. … That may mean physical therapy or something like that. Eventually, that gets to a hip replacement, a knee replacement, a shoulder replacement,” Lyras says. “For a good percentage of people, things wear out, just like a car needs new brakes or new oil.”
The decision to have surgery, the physicians agree, is left to the patient’s discretion. Doctors may make their recommendations but it’s up to patients to make the call.
“You tell me when you’re ready. People, for the most part, present to us with varying levels of care prior to seeing us. It’s when it gets to the point where it’s affecting their daily living and the things they want to do [that they decide to get surgery],” says Dr. Jeffrey Johnston, an orthopedic surgeon with Mercy Health-Youngstown.
To guide patients through an often-unfamiliar process, Trumbull Regional Medical Center has added a patient navigator to its suite of orthopedic services. Peggy Rable, a registered nurse, works as a conduit between patients and doctors to set up appointments, ensuring everything is ready for surgery – from lab results to CT scans – and following up with them after their operations.
“It eases their minds. After I’m done telling them everything, they feel so much better. They know what to expect, how pain will be controlled, what to ask for,” she says. “They’re much better prepared. They come in knowing that they’re going to stay with their daughter for a week before they go home and after they’re doing better. When they come in for pretesting, they’re given a book with information and some exercises to do.”

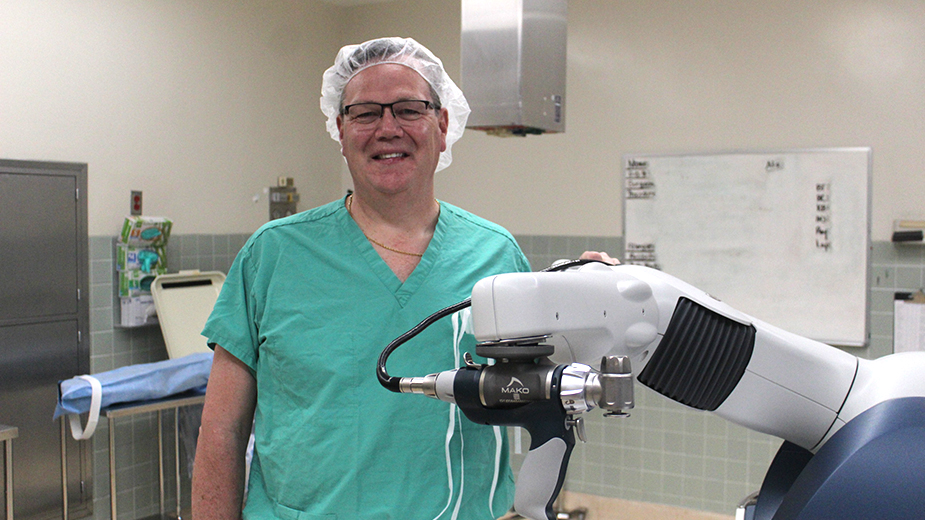
In the OR, robotics help surgeons achieve better outcomes. Among the standards in the Mahoning and Shenango valleys is the Mako robot, used at Trumbull Regional, Mercy Health’s St. Elizabeth Boardman Hospital and the Orthopaedic Surgery Center. Thanks to a CT scan of the site of the surgery before the operation, doctors can fit replacement joints with better accuracy, leading to more comfort for patients afterward.
“The Mako robot allows you to be much more accurate and as a result, because I don’t have to put a rod in, the incision is much smaller,” Trumbull Regional’s Jones explains. “I’ve noticed the range of motion has gotten much better. It’s all about making movements more natural. That happens because we can balance ligaments better and because the robot tells us, within a millimeter, where we’re going.”
While the Mako robot is primarily used on hip and knee replacements, Jones and Joseph expect the procedures in which it can be used to expand in coming years, including rotator cuff surgery and ACL repairs.
Care doesn’t end as soon as patients are discharged after surgery. At Hillside Rehabilitation Hospital, part of the Steward Health Care system alongside Trumbull Regional, therapists work with patients on customized plans to get them back to their pre-surgery mobility levels – or better. The hospital in Howland offers both outpatient therapy and inpatient rehabilitation.
“If a patient had total joint replacement, had some complications during surgery and just wasn’t able to progress fast enough to go home directly, they come to Hillside. When they’re here, they get therapy to build that mobility they need to return home independently so they can go to outpatient therapy,” says Jeffrey Koontz, director of rehabilitation services. “Especially for total knee [replacements], we’re looking for mobility. How far can they walk? Do they need a device? Have they progressed from a walker to a cane to no device? It’s about functional progression to return to the highest level of independence.”
With the Mahoning and Shenango valleys’ aging populations, the need for orthopedic care has increased. At Mercy Health-Youngstown, Dr. Ryan Foertch, director of the health-care system’s orthopedic service line, says volume has been steadily rising over the past few years and has involved every aspect of Mercy Health’s offerings.
“A lot of it starts with primary care physicians. Those are the first people who see a problem when it arises,” he says. “[Primary care doctors] always have specialists to rely on. … That’s where orthopedists work well with primary care physicians, physical therapists, podiatrists. That continuum of care is comprehensive and knowing what to do for injuries gets patients to where they need to be.”
The opening of the Orthopaedic Surgery Center in Boardman in 2019 was driven by the rising demand for outpatient surgeries, says chief operating officer Taylor Cera.
In the two years since, the center has added new specialties: women’s health, plastic and reconstructive surgery and eye surgery. While those fields aren’t within the traditional scope of orthopedics, they fit into its mission.
“Our mission is to improve the overall lifestyle of patients in our community. These specialties really embrace and expand our mission,” Cera says. “Right now, we’re focused on slow but calculated growth in terms of adding specialties that add high-volume procedures with a low complication rate.”
And at Southwoods Health, the growing demand has led to the system’s next endeavor – the construction of an orthopedic center at its Boardman campus. The system employs 11 orthopedists, spread across its footprint, says CEO Ed Muransky. The new site would consolidate those offices into a single, central office.
“It will allow someone with knee pain not just to see a doctor, but to be educated about what’s out there, what treatments are working,” Muransky says. “It’s similar to the pain and spine center we have now, which is more than just back surgery. “If you have shoulder pain from arthritis, what’s out there? Right now, it’s fragmented – even at Southwoods – across a number of locations.”
Pictured at top: With surgery typically the final option for orthopedic care, doctors at Trumbull Regional Medical Center often use the Mako robot for joint replacements, says Dr. Kenneth Jones, to reduce the size of the surgical site.