Community Needs Drive ‘Ongoing, Ever Evolving Planning’ for Virus
YOUNGSTOWN, Ohio — As hospital systems within the state work together and across state lines to address the novel coronavirus pandemic, one thing is clear to Dr. Amy Acton: “We are never going to work together quite the same.”
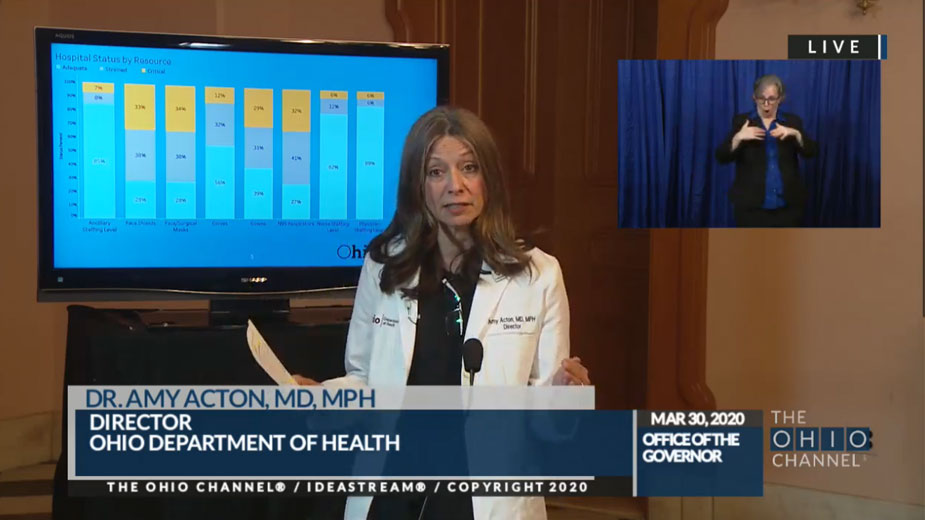
The director of the Ohio Department of Health addressed the planning process for the state’s response to COVID-19 – the disease spread by the coronavirus – which she says isn’t one-size-fits-all. Hospital systems have been working together to maximize care for all patients, she said during the state’s daily press briefing Monday, and their plans for dealing with the pandemic will evolve through the surge, after the surge “and after we return back to normal,” she said.
“No hospital system in the world has ever faced what we’re facing around the world with coronavirus,” Acton said. “So when we say ‘plans’, what we’re really doing is ongoing, ever evolving ‘planning.’ “
CEOs of the state’s hospital systems are collaborating to effectively use the resources throughout their branches in cities, as well as suburban and rural areas, to “create a master system” on how the industry maximizes its resources, Acton said. Industry leaders have worked closely with state and local health departments, nonprofits and civic leaders to ascertain the extent of those resources, from using nursing home beds differently, using hospital, hotel and dorm rooms differently, or exploring the possibility of using convention centers to house patients if needed, Acton said.
Currently, medical/surgical beds are at 54% occupancy and ventilators are at 30% occupancy, she said. The available infrastructure, however, needs to be doubled, she said.
At the Emergency Operating Center, Acton and her team are developing an “integrated, complex effort” in managing the strategic deployment of the state’s dwindling resources, particularly with personal protective equipment, or PPE, she said. Hospitals have “freed up a lot of equipment” by not doing elective surgeries, but usage of certain PPE items are at critical levels, particularly face shields, face/surgical masks, gowns and N95 respirators, she said.
Steps have been taken to alleviate the strain on those resources. Late Sunday evening, the U.S. Food and Drug Administration approved the full capability of technology produced by Battelle Memorial Institute in Columbus that, when ramped up to full production, will sterilize up to 80,000 masks per machine, said Lt. Gov. Jon Husted. Two machines will be placed in Ohio.
The nonprofit research company expects to sterilize 10,000 Tuesday and will ramp up its efforts as shipments of N95 respirators start coming in from hospitals around the state, he said.
“This is a major breakthrough for us in Ohio, but it’s also something where we’re taking Ohio technology and helping people in other states,” Gov. Mike DeWine said.
State prisons are working to produce PPE and have already made some 500 hospital gowns, DeWine reported. Once the prisons receive more fabric, they’ll be able to produce 44,000 more.
They’ll also be able to produce 5,000 surgical masks daily, with enough materials for up to 2 million, DeWine said. On April 14, the prisons will also receive ingredients to make some 1,400 gallons of hand sanitizer, and they are gearing up to make face shields.
Preparing the medical capacity “that we know we’re going to need as the COVID spread peaks” is the main effort of the Emergency Operating Center, said Maj. Gen. John C. Harris Jr., who works closely with Acton. The center is coordinating with regional leaders to ensure they are disbursing the appropriate resources where they are most needed, he said.
The center is weighing the possibilities of leasing buildings as needed or leveraging unused state facilities to increase hospital capacity, as well as constructing new buildings, Harris said. It’s also “turning over every rock possible” to find and collect PPE “because that is such an in-demand item right now,” he noted, and it stands ready to help with staffing.
“Because we know that the workforce is going to be stressed during these peak periods,” he said.
That includes deploying members of the National Guard, which has already been visible in the Mahoning Valley assisting with food drives and constructing tents outside of hospital emergency rooms. In the coming days, residents will “see service members in uniform in your community doing things in increasing numbers in the very near future,” he said.
In addition to conducting site assessments, they will be acting as liaison with regional leaders and reporting the community’s exact requirements back to the center, he said.
“Every person is a participant in this,” Harris said. “Your individual actions are critical in ensuring we continue to flatten the curve.”
Current modeling estimates the surge of COVID-19 cases in Ohio will peak on April 25, at which point the state will be seeing nearly 10,000 new cases daily.
The Emergency Operating Center is working to help hospitals deal with that surge by removing barriers when possible and expediting medical students to get them in a position to help, Acton said. Those efforts include online trainings to help train nursing students or nurses who have been in other fields to work needed positions, she said. Training can also allow surgeons to take on more nursing duties. The state is also looking to graduate medical students early so they can be deployed to the front lines of the crisis, she said.
Acton and her team have been working with medical schools to develop a curriculum to train earlier year medical and nursing students to be “amateur disease detectives,” she said. When testing is put in place, these students will be able to help identify those who are infected, as well as conducting contact tracing.
For medical students, this will be “a turning point in their careers,” as many of them have already had experience in hospitals, so “there’s nothing keeping them from doing the work now,” Acton said.
“We’re going to actually need literally boots on the ground folks, far beyond anything public health has even had on their payrolls, to be able to do that and be able to do that as quickly as possible,” she said.
The DeWine administration has been communicating with governors in states surrounding Ohio as well to establish contingency plans when resources need to be shared across state lines, the governor said.
For homeless populations, the Ohio Department of Mental Health is offering guidance on how homeless shelters, group homes, recovery houses and other shelters can address those populations, DeWine said.
“Shelters are not built for social distancing. And they present unique problems and challenges,” he said.
To address those issues, the state has assembled a team comprised of the Coalition on Housing and Homelessness in Ohio, the Ohio Chapter of the National Alliance on Mental Illness and Ohio Recovery Housing to provide guidelines to shelters, DeWine said. They’ll work to include those populations in the state’s overall coronavirus response plan using community health centers, as well as plans for quarantine when needed.
Shelters with questions about CDC guidelines and other information can email COVID19Housing@mha.ohio.gov.
Copyright 2024 The Business Journal, Youngstown, Ohio.